The drug supply is evolving again. Just when public health agencies and harm reductionists were starting to wrap their heads around xylazine and nitazene, a new veterinary sedative has entered the scene: medetomidine. It's stronger, less predictable, and even more dangerous.
What Is Medetomidine, and Why Is It in the Fentanyl Supply?
Medetomidine is a powerful alpha-2 adrenergic agonist used in veterinary medicine, typically to sedate animals for surgery. It's not approved for human use. In early 2024, Toronto’s Drug Checking Service began detecting medetomidine in street-level fentanyl samples. By mid-2025, it had shown up in major U.S. cities including Philadelphia, Pittsburgh, Chicago, and San Francisco.
This isn’t just a new contaminant, it’s a game changer. Medetomidine is significantly more potent than xylazine. According to the DEA, it may be 200 to 300 times stronger, which dramatically increases the risk of overdose and death.
The Real Problem: It’s Invisible and Unresponsive to Naloxone
One of the biggest dangers of medetomidine is that it doesn’t respond to naloxone. When users experience an overdose, even prompt administration of Narcan may not be enough. In Chicago, a cluster of overdoses in 2024 showed patients with dangerously low heart rates and poor oxygen levels who didn’t respond to opioid reversal protocols.
Instead, the only effective intervention in many of these cases is respiratory support: bag valve masks, supplemental oxygen, and immediate emergency care. And because users can’t see or smell this contaminant, they’re often blindsided.
The Withdrawal Nightmare: A New Kind of Hell
Recent reports have uncovered a terrifying new dimension to this crisis: the withdrawal. Unlike opioid withdrawal, which is agonizing but rarely fatal, medetomidine withdrawal is proving to be a medical emergency of its own.
According to new reporting from The New York Times, users trying to detox are experiencing severe "autonomic hyperactivity." This isn't just the shakes; it’s a life-threatening storm of symptoms including dangerously high blood pressure, extreme tachycardia (rapid heart rate), hallucinations, and severe tremors.
Frontline medical providers are finding that standard detox protocols—and even the methods used for xylazine—are failing. Medications like methadone, buprenorphine, and standard doses of clonidine often aren't enough to stabilize these patients. Many are ending up in the ICU, requiring infusions of dexmedetomidine (a related hospital-grade sedative) just to keep their heart rates from skyrocketing. This complex withdrawal creates a "trap" for users, making it nearly impossible to stop using without high-level medical intervention.
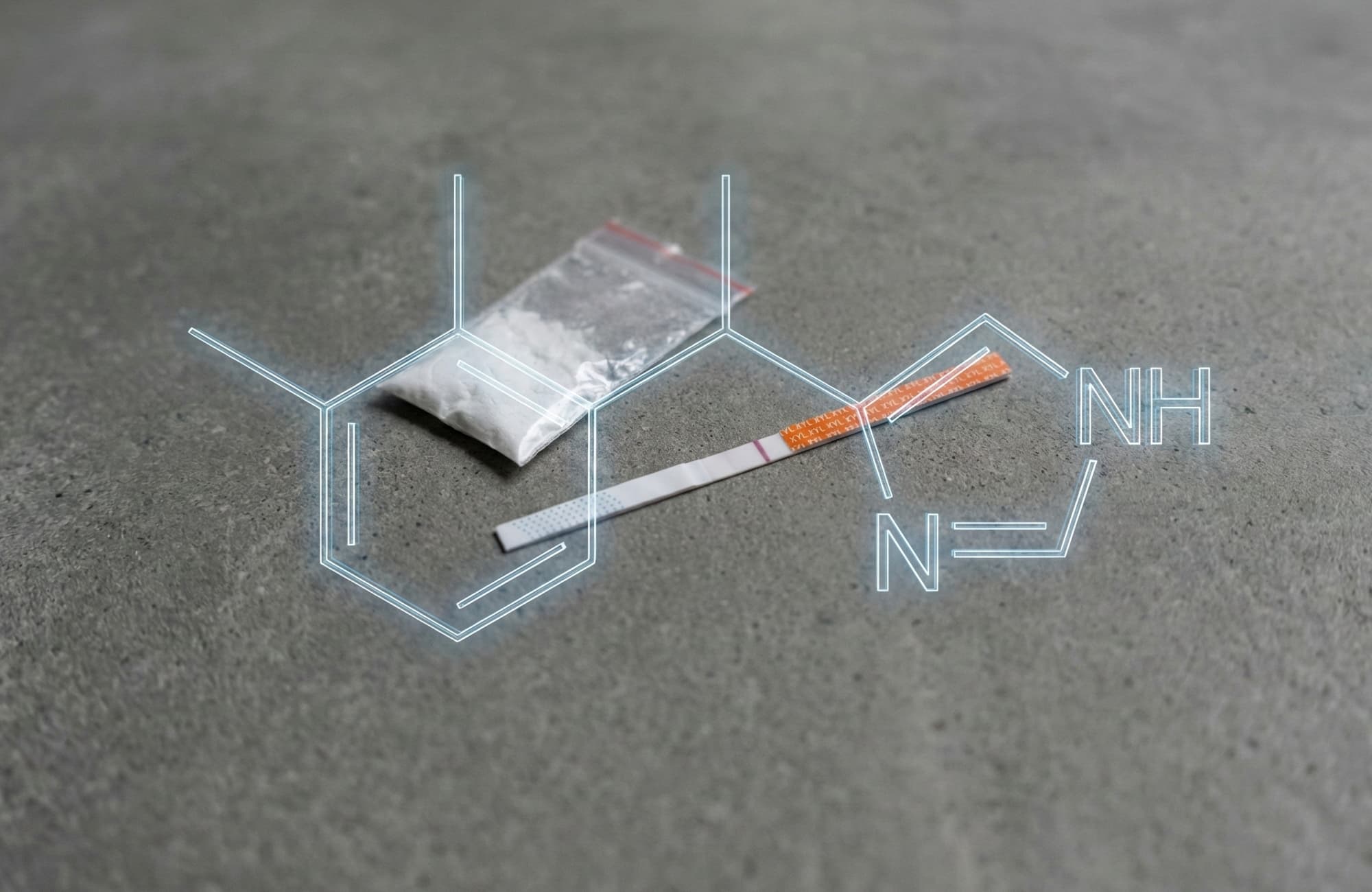
Test Strips Are Catching Up, But Gaps Remain
Until very recently, standard test strips left users flying blind against this new threat. Fortunately, the landscape is shifting. BTNX has released Rapid Response™ Medetomidine Test Strips specifically designed to detect this compound (and its active isomer, dexmedetomidine) with a cutoff of 1000 ng/mL. This is a massive step forward, but a word of caution: Xylazine test strips will NOT detect medetomidine. You need the specific strip for the specific adulterant.
While new strips are becoming available, they aren't yet in every harm reduction kit or head shop. Distribution takes time! We're eager to evaluate these strips and make them available for sale in the future through The Bunk Police site (stay posted). Note: Even with a positive strip result, you won't know the concentration or what else might be in the mix. That’s where lab-based drug checking remains essential.
In the city of Toronto, consistent lab testing has revealed how common these adulterants are. In a recent two-week report, 54% of fentanyl samples were adulterated with other sedatives or opioids, including medetomidine. This is a systemic problem, and it’s worsening.
Why Is This Happening Now?
The scheduling of xylazine in the U.S. may have triggered a shift. Suppliers looking for similar effects are now turning to unscheduled alternatives. Medetomidine fits the effects profile. It creates profound sedation, increases the perceived potency of fentanyl, and is readily available from overseas labs.
As long as enforcement focuses on banning one compound at a time, illicit chemists will stay one step ahead. Without comprehensive testing and real-time monitoring, we’re always reacting too late.
Harm Reduction Has to Evolve
We’re in a new era of synthetic adulterants. Here’s what that means for frontline harm reduction:
- Naloxone alone isn’t enough. Harm reduction kits need to include guidance on recognizing non-opioid overdoses and how to perform rescue breathing.
- Medical Advocacy is key. Users and advocates need to know that medetomidine withdrawal requires specific, often ICU-level care. Telling ER staff that "this might be medetomidine" could save a life by steering treatment toward alpha-2 agonists rather than just opioids.
- Update your testing toolkit. If you can access the new BTNX medetomidine strips, use them. But remember: a negative result on a xylazine strip does not mean your supply is safe from sedatives.
- Information must flow faster. Cities like Philadelphia and Toronto are leading the way by sharing toxicology data across EMS, hospitals, drug checking services, and public health departments. This needs to be the norm, not the exception.
- Users deserve transparency. If someone chooses to use, they should have access to accurate, up-to-date information about what they’re taking. That starts with testing and continues with education.
The Bunk Police Perspective
For over a decade, we’ve warned people about unknown substances in the supply. From RC benzos to cathinones, to fentanyl analogues no one's ever heard of, we’ve been there trying to identify and share information quickly. Medetomidine is another chapter in this story, but it’s also one of the most dangerous yet.
We believe everyone deserves access to clean data, clear tools, and the ability to make informed choices. We proudly offer worldwide access to lab-based drug checking services via Transparency Testing. Our team will continue to connect the dots between labs, mutual aid networks, and grassroots harm reduction organizations with improved access.
References
- DEA National Illicit Substances Report – Medetomidine Potency Center for Forensic Science Research & Education (CFSRE) – Public Alert: Medetomidine (May 2024)
- CDC Report on Chicago Overdose Cluster CDC MMWR: Overdoses Involving Medetomidine Mixed with Opioids — Chicago, Illinois, May 2024
- Toronto Drug Checking Report Toronto’s Drug Checking Service – Medetomidine Alerts & Reports
- News Coverage: San Francisco’s First Medetomidine Fatality San Francisco Chronicle – Drug Overdose Crisis & Emerging Threats
- Philadelphia Department of Public Health Bulletin Philly Health Alerts – Medetomidine: What You Need to Know
- Medetomidine Withdrawal Symptoms and Treatment Protocols The New York Times – Medetomidine Withdrawal Symptoms Treatment